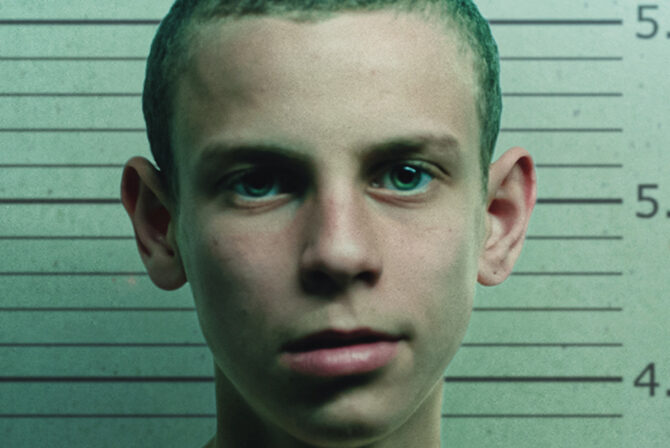
The first time I saw our son being led out of our house in handcuffs was when he was 17 years old, three months shy of his high school graduation. On an early spring night, my husband and I stood in our front doorway, watching as two police officers bundled our son into the back seat of the patrol car. Quickly they sped off, lights blazing but sirens thankfully silent, to drive him to the psychiatric unit of the hospital. My husband and I walked back inside, sat down on the nearest chairs, too stunned to talk.
Our son’s behavior had been spiraling out of control for months. We had pleaded with him, argued with each other, pleaded with him and then returned to arguing. He wasn’t listening to us, and my husband and I could hardly bear to listen to each other, so far apart were we in our thinking.
“It will get better,” my husband said, “This is just a stressful phase.”
“I don’t think so,” I told him, “This is beyond stress. I’m afraid of what might happen next.”
READ: Mayim Bialik: Why I Support This Mental Health Organization & You Should Too
And when the vindictive comments became raging anger and the raging anger turned into threats, that night when it all erupted, we called our son’s psychiatrist who suggested we call the police. I knew to ask for officers with mental health training. The older officer had a calm presence and his young female partner spoke in a soothing voice. Our son grew less hostile as they spoke with him. He cooperated and readily gathered up his clothes and his backpack, as if he were going to school.
But he wasn’t. They don’t put you in handcuffs for carpool.
We arrived at the hospital late that night. The reception desk directed us to the locked door of the “mental health” unit where we had to press the button to be admitted. A social worker introduced herself, and led us to a corner of the waiting room where she, casually dressed, impassive faced, wearily asked us questions and duly took notes of our responses.
READ: It’s Time to Fight the Stigma of Mental Illness
Those were the high (or low) points. Then the social worker left us until morning and my husband and I settled in to doze through the rest of the night in those soon-to-become-very-familiar hard orange plastic chairs. Our son spent that night in another room down the hall, with the door left open and the overhead light on all night so he could be easily observed by the nurses. He refused to talk to us.
The hope that rose up in me that first night , that this was a promptly fixable medical problem, has long since been replaced by reality.
We have seen other police officers come into our home, have spent many hours on those waiting room chairs, been woken up by frantic phone calls, and lived through the failures of overly-optimistic treatment programs and the false promises of new medications.
As the months became years, I have become an involuntary expert.
READ: The Day I Had to Tell My Son He Was Different
I applied my lawyerly persistence to press for solutions in the overly-complex, often inhumane, mental health system. Fighting through my frustration with doctors, therapists, insurance companies and pharmacists was the easy part.
Much harder was trying not to take it personally when our son, in his late teens and early twenties, frequently hurled vile invectives at me. His ugly words intended to deeply hurt me did so. He often told me, without any basis, that I, his Mom who had nurtured him, understood him, was the sole cause of his problems.
As the nasty phrases tumbled out of his mouth, there were many days when I loved our son but did not like him at all. The sympathy I had felt in the early days of his struggles waned. I grew angry: with him, with the many doctors, one after another, who could not find treatments that helped. Part mental illness, part behavioral, his is a complex mix that no doctor could readily grasp.
READ: It’s Time to Talk About Therapy
“He’s so brilliant,” the doctors and therapists would tell me.
“I know.” I would respond.
“If only he was less smart and more compliant.”
“If only,” I would agree.
A few years after that first hospitalization our son came back home to live with us, to return to college. At first he seemed engaged in his courses, we were warily hopeful. Then the familiar pattern of anger and irritability emerged. He tinkered with his meds. He disagreed with his psychiatrist. He argued with his professors. He rattled his classmates. His behavior became erratic.
One night he burst into the house after an evening class, on a tear, upset with everyone. We were in our regular places in the family room. I was on the couch doing my nearly finished needlepoint of a calming coastal scene; needlepoint I wasn’t very good at but indulged in because my mother had done it before me.
READ: Managing Motherhood & Depression Means Asking For Help
Our dogs lay dozing next to me as our son began his monologue of vitriol.
We tried to soothe him. He wasn’t listening. Whatever we said only enraged him more. Suddenly he grabbed the needlepoint canvas out of my hands, ran into the kitchen, turned on a gas burner on the stove, and held the canvas above it until it went up in flames.
“No, no, stop, please stop, don’t do that!”
I could not move from my seat on the couch.
Next he went into the living room, found the antique bottles that had belonged to my mother before she died; he knew how much I treasured them. He smashed them to the floor, then picked up some of her vintage plates and threw them against the wall.
READ: Whirling Together out of the Darkness
Then more door slamming, harsh words exchanged, before he went to the basement and barricaded himself in. The next morning he left our house again. Involuntarily.
A decade has passed since that that first hospitalization. Five years have gone by since the night he destroyed the tangible memories of my mother. The warmth that I felt towards our son has faded. I love him, but I no longer care as deeply as I once did. The caring had cost me too much of myself.
Our son still struggles, my husband and I still disagree but the mega-rollercoaster that our lives were for many years has slightly slowed its speed. In its wake I have become more empathetic to the sorrows of others. Every day worries glide right past me.
I try to stay positive, to put my involuntary expertise to good use. I started a support group called “parents of young adults who struggle” at my synagogue, now five years strong. I am on the board of a mental health non-profit, I advise other parents, I write articles to inform them–mental illness can happen to your young adult son or daughter, here’s what to do, here’s what not to do–and here’s what you may want to do–but it likely won’t work, trust me on that.